Health Activations
Engage, Retain, Thrive.

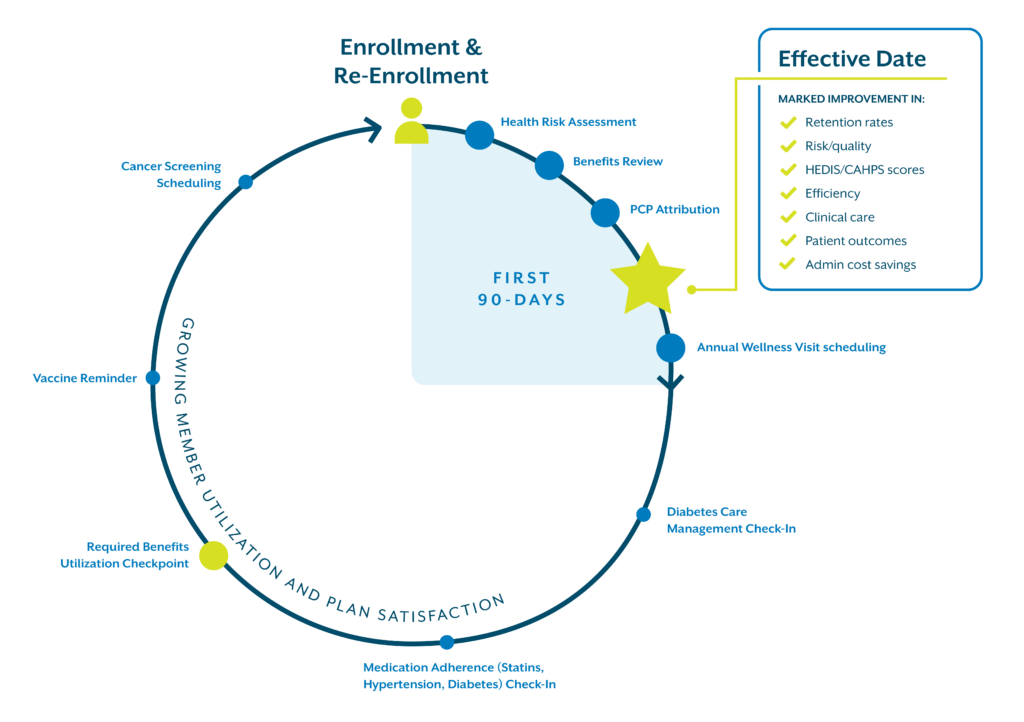
Nurture relationships before, during, and after the start of benefits. Invest in engagements that promote member satisfaction, improve important measures, and keep you competitive in today’s challenging market.
Member Health is Your Health
Be rewarded by doing the exact right thing, at the exact right time, for your members. We can enhance the member journey with activities that promote:
Your Goals, Our Programs
We take your specific plan goals into account, offering programs tailored to helping you achieve the best outcomes possible, all aimed at cost savings and revenue generation.
Ready to explore Bloom Health Activations?
Download our fact sheet.
Discover the 90-day difference.
Our Health Activations programs engage members at the point of sale and before their effective date, giving you a head start on achieving plan-year goals up to 90 days sooner.
Health Activations: Measuring Impact
Bloom Health Activations maximize your sales-marketing efforts and foster member relationships that last. Here are just a few of the positive changes we’ve been able to make for our Health Activation clients.
Reduced Cancellations
60%
When completing an HRA post-application and adding Annual Wellness Visit scheduling
Decreased Rapid Disenrollment
25%
Using both Welcome Call & Plan/Supplemental Benefit Review
Improved Impacted Metric
3/4
Bloom managed PBPs year over year
HRA Completion rate
90%
of new members within 90 days of enrollment